1.Pulmonology:
A) Link to patient details:
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's probl Evolution of symptomatology
*1st episode of sob - 20 yr back
* 2nd episode of sob - 12 yr back
* From then she has been having yearly episodes for the past 12 yrs
* Diagnosed with diabetis - 8yrs back
* Anemia and took iron injections - 5yr ago
* Generalised weakness - 1 month back
* Diagnosed with hypertension - 20 days back
* Pedal edema - 15 days back
* Facial puffiness- 15 yrs back
* Anatomical location of problem - lungs
* Primary etiology of patient- usage of chulha since 20 yrs might be due to chronic usage
2)what r the mechanism of action indication and efficacy over placebo of each of the phramacological and nonphramacological interventions used for this patien
*Head end elevation :
MOA;
*.improves oxygenation
.*decreases incidence VAP
.*increases hemodynamic performance
.*increases end expiratory lung volume
*.decreases incidence of aspiration
#Indication: .head injury
.meningitis
.pneumonia
~ oxygen inhalation to maintain spo2
~Bipap:non invasive method
#MOA
:Assist ventilation by delivering positive expiratory and inspiratory pressure with out need for ET incubation9
3. Cause for current acute excerbation -
it could be due any infection
4.could the ATT affected her symptoms if so how?
Yes ATT affected her symptoms
Isoniazid and rifampcin ---.>nephrotoxic -- > raised RFT was seen in this pt sugest the effect of ATT
2.Neurology:
A) Link to patient details:
1) what is the evolution of the symptomology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans: The patient is a chronic alcoholic, he drinks about 3-4quarters/day.he had developed seizures following the cessation of alcohol for 24hours it is due to the following reason:-alcohol affects the way in which nerve cells communicate. receptors are specialized proteins on the surface of nerve cells that receive chemical signals from one another. With long-term alcohol consumption, receptors affected by alcohol undergo adaptive changes in an attempt to maintain normal function.
Two important brain communication systems affected by alcohol involve the neurotransmitters:gamma-aminobutyric acid and glutamate.
The GABA system:
GABA is an inhibitory neurotransmitter that helps to regulate brain function by rendering nerve cells less sensitive to further signaling. single doses of alcohol facilitate the inhibitory function of the GABA receptor, contributing to alcohol intoxicating effects. During withdrawal, brain GABA levels fall below normal and GABA activity declines. The combination of reduced brain GABA levels and GABAa receptor sensitivity may be contributed an adaptation to the presence of alcohol. In the absence of alcohol, the resulting decrease in inhibitory function may contribute to Symptoms of nervous system hyperactivity associated with both acute and protracted AW.
The glutamate system:
The major excitatory neurotransmitter in the brain is glutamate, which communicates with three major subtypes of glutamate receptors. Among these, the N-methyl-D-aspartate (NMDA) receptor plays a role in memory, learning, and the generation of seizures. Alcohol inhibits the excitatory function of the NMDA receptor in laboratory studies at concentrations associated with mild to moderate alcohol intoxication in humans. As with the increased inhibitory function of the GABAA receptor, the decreased excitatory function of the NMDA receptor is consistent with alcohol’s general sedative effect. Long-term alcohol administration produces an adaptive increase in the function of NMDA receptors. Acute AW activates glutamate systems. In turn, AW seizures are associated with increased NMDA receptor function. Persistent alterations in NMDA receptor function may potentiate the neurotoxic and seizure-inducing effects of increased glutamate release during withdrawal.
The symptom: irrelevant talking, decreased food intake, tremors, sleep disturbance is due to the following reason: chronic alcohol consumption causes thiamine deficiency due to impaired absorption of thiamine from the intestine, a possible genetic predisposition, inadequate diet, reduced storage of thiamine in the liver and other nutritional deficiencies.
THE PATHOPHYSIOLOGY:
Thiamine, one of the first B vitamins to be discovered also known as Vitamin B1, is a coenzyme that is essential for intricate organic pathways and plays a central role in cerebral metabolism. This vitamin acts as a cofactor for several enzymes in the Krebs cycle and the pentose phosphate pathway, including alpha-keto-glutamic acid oxidation and pyruvate decarboxylation. Thiamine-dependent enzymes function as a connection between glycolytic and citric acid cycles. Therefore, deficiency of thiamine will lead to decreased levels of alpha-keto-glutarate, acetate, citrate, acetylcholine and accumulation of lactate and pyruvate. This deficiency can cause metabolic imbalances leading to neurologic complications including neuronal cell death. Neuronal death in the mammillary bodies and thalamus were implicated in multiple cases of Wernicke encephalopathy studied. Studies involving computed tomography (CT) and magnetic resonance imaging (MRI) of patients with Wernicke encephalopathy revealed lesions in the thalamus with dilated ventricles and volume loss in the mammillary bodies. The lesions are usually symmetrical in the midbrain, hypothalamus, and cerebellum.
The kidneys have an important job as a filter for harmful substances .alcohol causes changes in the function of the kidneys and makes them less able to filter the blood .alcohol also affects the ability to regulate fluid and electrolytes in the body. In addition, alcohol can disrupt hormones that disrupt hormones that affect kidney function .people who drink too much are more likely to have high blood pressure. High blood pressure is a common cause of kidney disease. The increase in levels of urea, creatinine, uric acid leads to uraemic encephalopathy. which causes asterixis.
the deficiency of thiamine and increase in levels of toxins in the body due to renal disease is the primary etiology of the patient's problem.
2)what are the mechanism of action, indication, and efficacy over placebo of each of the pharmacological and nonpharmacological interventions used for this patient?
Ans: I) Thiamine helps the body cells change carbohydrates into energy. It has been used
as a supplement to cope with thiamine deficiency
ii)Lorazepam binds to benzodiazepine receptors on the postsynaptic GABA-A ligand-gated chloride channel neuron at several sites within the central nervous system.it enhances the inhibitory effects of GABA, which increases the conductance of chloride ions into the cell
iii)pregabalin subtly reduces the synaptic release of several neurotransmitters, apparently by binding to alpha2-delta subunits, and possibly accounting for its actions invivo to reduce neuronal excitability and seizures.
iv)Lactulose is used in preventing and treating clinical portal-systemic encephalopathy .its chief mechanism of action is by decreasing the intestinal production and absorption of ammonia.
v)Potchlor liquid is used to treat low levels of potassium in the body.
3)why have neurological symptoms appeared this time, that were absent during withdrawal earlier ? what could be a possible cause for this time?
Due to excess thiamine deficiency and excess toxins accumulation due to renal disease caused by excess alcohol addiction.
4)what is the reason for giving thiamine in this patient?
chronic alcohol consumption causes thiamine deficiency due to impaired absorption of thiamine from the intestine,Thiamine, one of the first B vitamins to be discovered also known as Vitamin B1, is a coenzyme that is essential for intricate organic pathways and plays a central role in cerebral metabolism. This vitamin acts as a cofactor for several enzymes in the Krebs cycle and the pentose phosphate pathway, including alpha-keto-glutamic acid oxidation and pyruvate decarboxylation. Thiamine-dependent enzymes function as a connection between glycolytic and citric acid cycles. Therefore, deficiency of thiamine will lead to decreased levels of alpha-keto-glutarate, acetate, citrate, acetylcholine, and accumulation of lactate and pyruvate. This deficiency can cause metabolic imbalances leading to neurologic complications including neuronal cell death.
5)what is the probable cause for kidney injury in this patient?
The kidneys have an important job as a filter for harmful substances .alcohol causes changes in the function of the kidneys and makes them less able to filter the blood .alcohol also affects the ability to regulate fluid and electrolytes in the body. In addition, alcohol can disrupt hormones that disrupt hormones that affect kidney function .people who drink too much are more likely to have high blood pressure. High blood pressure is a common cause of kidney disease.
6)what is the probable cause for the normocytic anaemia?
alcohol causes iron deficiency or iron overload due its affect on production of new blood cells organs i.e,bonemarrow and the metabolism of iron .alocohol causes a affect on progenitor cells of blood causing decreased WBC .RBC.alochol decreases iron absorption from intestine .
7)could chronic alcohlism have aggravated the foot ulcer formation ?if yes and why ?
yes,As the patient is diabetic the chance of ulcer formation increases .in a patient of chronic alcoholic theimmune system is weak due to the affect on blood cells formation and iron absorption.due to this healing of an ulcer dampens.
B) Link to patient details:
1) What is the evolution of the symptomology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patients problem?
ANS. Timeline of the patient is as follows-
7 days back- Patient gave a history of giddiness that started around 7 in the morning; subsided upon taking rest; associated with one episode of vomiting
4 days back- Patient consumed alcohol; He developed giddiness that was sudden onset, continuous and gradually progressive. It increased on standing and while walking.
H/O postural instability- falls while walking
Associated with bilateral hearing loss, aural fullness, presence of tinnitus
Associated vomiting- 2-3 episodes per day, non projectile, non bilious without food particles
Present day of admission- Slurring of speech, deviation of mouth that got resolved the same day
Anatomical location- There is a presence of an infarct in the inferior cerebellar hemisphere of the brain.
Etiology- Ataxia is the lack of muscle control or co-ordination of voluntary movements, such as walking or picking up objects. This is usually a result of damage to the cerebellum (part of the brain that controls muscle co-ordination)
Many conditions cause cerebellar ataxia- Head trauma, Alcohol abuse, certain medications eg. Barbituates, stroke, tumours, cerebral palsy, brain degeneration etc.
In this case, the patient has hypertension for which he has been prescribed medication that he has not taken. Stroke due to an infarct can be caused by blockade or bleeding in the brain due to which blood supply to the brain is decreased, depriving it of essential oxygen and nutrients. This process could’ve caused the infarct formation in the cerebellar region of the brain, thus causing cerebellar ataxia.
2) What are the mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS.
A) Tab Vertin 8mg- This is betahistine, which is an anti- vertigo medication
MOA- It is a weak agonist on H1 receptors located on blood vessels of the inner ear. This leads to local vasodilation and increased vessel permeability. This can reverse the underlying problem.
Indications- Prescribed for balance disorders. In this case it is used due to patients history of giddiness and balance issues.
B) Tab Zofer 4mg- This is ondanseteron- It is an anti emetic
MOA- It is a 5H3 receptor antagonist on vagal afferents in the gut and they block receptors even in the CTZ and solitary tract nucleus.
Indications- Used to control the episodes of vomiting and nausea in this patient.
C) Tab Ecosprin 75mg- This is aspirin. It is an NSAID
MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and thromboxane synthesis
Indications- They are anti platelet medications and in this case used to prevent formation of blood clots in blood vessels and prevent stroke.
D) Tab Atorvostatin 40mg- This is a statin
MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and degeneration. Hence plasma LDL level decreases.
Indications- Used to treat primary hyperlipidemias. In this case it is used for primary prevention of stroke.
E) Clopidogrel 75mg- It is an antiplatelet medication
MOA- It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
Indications- In this case it decreases the risk of heart disease and stroke by preventing clotting
F) Thiamine- It is vitamin B1
It is naturally found in many foods in the human diet. In this case, the patient consumes excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of essential vitamins due to impaired ability of the body to absorb these vitamins.
Indications- Given to this patient mainly to prevent Wernickes encephalopathy- that can lead to confusion, ataxia and opthalmoplegia.
G) Tab MVT- This is methylcobalamin
Mainly given in this case for vitamin B12 deficiency.
3) Did the patients history of denovo hypertension contribute to his current condition?
ANS. A cerebellar infarct is usually caused by a blood clot obstructing blood flow to the cerebellum. High blood pressure that is seen in hypertension (especially if left untreated) can be a major risk factor for the formation of cerebellar infarcts.
Increased shear stress is caused on the blood vessels. The usual adaptive responses are impaired in this case, thus leading to endothelial dysfunction in this case. High BP can also promote cerebral small vessel disease. All these factors contribute to eventually lead to stroke.
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic stroke?
ANS. Meta analysis of the relation between alcohol consumption and increased risk of stroke has mainly weighed in to the formation of two types- ischaemic and haemorrhagic stroke.
Ischaemic stroke- this is more common. This Is caused by a blood clot blocking the flow of blood and preventing oxygen from reaching the brain
Haemorrhagic stroke- occurs when an aneurysm bursts or when a weakened blood vessel leaks, thus causing cerebral haemorrhage
According to a Cambridge study, heavy drinkers have 1.6 more chance of intracerebral haemorrhage and a 1.8 increased chance of subaracnoid haemorrhage. The adverse effect on BP that is seen due to increased drinking is a major stroke risk factor and increase the risk of heart stroke.
Many studies show that with mild and moderate drinking . the risk of ischaemic stroke decreases due to decreased level of fibrinogen which helps in the formation of blood clots. However, heavy alcohol intake is associated with impaired fibrinolysis, increased platelet activation and increased BP and heart rate.
So In this case, his history of alcoholism, coupled with his hypertension definitely could be a causative factor of his current condition.
C) Link to patient details:
1.What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) *Evolution of symptoms :patient was normal 8 months back then developed b/l pedal edema which gradually progressed.
Aggerevated in sitting and standing position, relived on taking medication
*Palpitations :since 5days, sudden in onset which is more during night
Aggerevated by lifting heavy weights, speaking continuously
*Dyspnoea during palpitations (NYHA-3) since 5 days
*pain:since 6days, radiating along left upper limb, more during palpitations and relived on medication.
Chest pain associated with chest heaviness since 5 days
Anatomical localisation :
Palpitations
Dyspnoea(NYHA-3)
Pedal edema
Chest pain
Radiating pain along her left upper limb
Etiological agent :
*By localization, electrolyte imbalance (hypokalemia) causing the her manifestations like palpitations, chest heaviness, generalised body weak ness
*radiating pain along her left upper limb due to cervical spondylosis
2Q) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
A) Reason: recurrent hypokalemic periodic paralysis
Current risk factor:due to use of diuretics
Other risk factors
A) Abnormal loses:
Medications-diuretics, laxatives, enema, corticosteriods
Real causes- osmotic diuresis, mineralo corticoid excess, renal tubular acidosis, hypomagnesenemia
B) trance cellular shift : alkalosis, thyrotoxicosis, delirium tremans, head injury, Myocardial, ischemia, recurrent hypokalemic periodic paralysis
C) Inadequate intake: anorexia, dementia, stareation, total parental nutrition
D) psuedohypokalemia:delayed sample analysis, significant leukocytosis
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
A) changes seen in ECG :
Earliest change :decreased T-wave amplitude, ST depression, Twave - and inversion or flat;prolonged PR interval;presence of Uwaves
In Severe cases :ventricular fibrillation, rarely AV block
Symptoms of hypokalemia :
Weakness & fatigue, palpitations, muscle cramps & pain, anxiety, psychosis, depression, delirium.
D) Link to patient details:
https://rishikoundinya.blogspot.com/2021/05/55years-old-patient-with-seizures.html
QUESTIONS:
1.Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
seizures after ischaemic strokes. An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarisation, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypoperfusion, and hyperperfusion injury
Seizures after haemorrhagic strokes are thought to be attributable to irritation due to (hemosideri. Deposits)caused by products of blood metabolism
Late onset seizures are associated with the persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Initially the patient might have had Simple partial seizures (no loss of consciousness) and might have progressed to Generalised Tonic Clonic seizures (loss of consciousness)
E) Link to patient details:
https://nikhilasampathkumar.blogspot.com/2021/05/a-48-year-old-male-with-seizures-and.html?m=1
Questions: 1) What could have been the reason for this patient to develop ataxia in the past 1 year?
The patient has minor unattended head injuries in the past 1 yr. Accoding to the CT scan, the patient has cerebral haemorrhage in the frontal lobe causing probably for the occurrence of Frontal lobe present should have been cured on their own. But the patient is a chronic alcholic. This might have hindered the process of healing or might have stopped the healing rendering it to grow further more into 13 mm sized hemorrhages occupying Frontal Parietal and Temporal lobes
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
The patient has minor unattended head injuries. During the course of time the minor hemorrhages if present should have been cured on their own. But the patient is a chronic alcholic. This might have hindered the process of healing or might have stopped the healing rendering it to grow further more into 13 mm sized hemorrhages occupying Frontal Parietal and Temporal lobes
F) Link to patient details:
http://shivanireddymedicalcasediscussion.blogspot.com/2021/05/a-30-yr-old-male-patient-with-weakness.html
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
The closeness of facial bones to the cranium would suggest that there are chances of cranial injuries. Since the Zygomatic arch and Mandibular process is very close to the cranium, this might play a role in the patient's present condition
2.What are warning signs of CVA?
Weakness or numbness of the face, arm or leg, usually on one side of the body
Trouble speaking or understanding
Problems with vision, such as dimness or loss of vision in one or both eyes
Dizziness or problems with balance or coordination
Problems with movement or walking
Fainting or seizure
Severe headaches with no known cause, especially if they happen suddenly
3.What is the drug rationale in CVA?
Mannitol- Because of its osmotic effect, mannitol is assumed to decrease cerebral edema. Mannitol might improve cerebral perfusion by decreasing viscosity, and as a free-radical scavenger, it might act as a neuroprotectant.
Ecospirin
For the prevention of heart attack, stroke, heart conditions such as stable or unstable angina (chest pain) due to a blood clot.
Atrovas-Atorva 40 Tablet belongs to a group of medicines called statins. It is used to lower cholesterol and to reduce the risk of heart diseases. Cholesterol is a fatty substance that builds up in your blood vessels and causes narrowing, which may lead to a heart attack or stroke.
Rt feed RT feed is a nursing procedure to provide nutrition to those people who are either unable to obtain nutrition by mouth or are not in a state to swallow the food safely.
4. Does alcohol has any role in his attack?
When the patient met with an accident there might be cranial damage which was unnoticed.
If so his occasional drinking may or may not have hindered the process of the minor hemorrhages getting healed and might have caused this condition
But since the patient is not a chronic alcoholic and so Alcohol might not have played any role.
Therefore it cannot be evaluated without further details
5.Does his lipid profile has any role for his attack??
The inverse relationship between serum HDL-C and stroke risk . When taken together it seems clear that higher baseline levels of serum HDL-C lower the risk of subsequent ischemic stroke.
G) Link to patient details:
2.what is finger escape?
Finger escape
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi. . This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign".
3.what is Hoffman's sign?
Hoffman's sign or reflex is a test used to examine the reflexes of the upper extremities. This test is a quick, equipment-free way to test for the possible existence of spinal cord compression from a lesion on the spinal cord or another underlying nerve condition
H) Link to patient details:
1) What can be the cause of her condition ?
Ans; Presence of cortical vein thrombosis with hemorrhagic venous infarction in right posterior temporal lobe and also Iron deficiency anaemia
2) What are the risk factors for cortical vein thrombosis?
Ans; For children and infants Problems with the way their blood forms clots
Sickle cell anemia
Chronic hemolytic anemia
Beta-thalassemia major
Heart disease — either congenital (you're born with it) or acquired (you develop it)
Iron deficiency
Certain infections
Dehydration
Head injury
For newborns, a mother who had certain infections or a history of infertility
For adults
Pregnancy and the first few weeks after delivery
Problems with blood clotting; for example, antiphospholipid syndrome, protein C and S deficiency, antithrombin III deficiency, lupus anticoagulant, or factor V Leiden mutation
Cancer
Collagen vascular diseases like lupus, Wegener’s granulomatosis, and Behcet syndrome
Obesity
Low blood pressure in the brain (intracranial hypotension)
Inflammatory bowel disease like Crohn’s disease or ulcerative colitis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Ans Missed medication
Lack of sleep
Stress
Menstruation About half of women of childbearing age with epilepsy have increased seizures around their period. This is most likely due to hormonal changes that occur during your monthly cycle.
Herbal medications — as well as the herbs that go into many dietary supplements — can actually cause seizures or worsen side effects of seizure medication. The same goes with essential oils. Certain ones, such as juniper and umbrella plant, have been known to induce seizures.
Vitamin B6 (pyridoxine) deficiency is the only type of vitamin deficiency that’s been proven to potentially cause or worsen seizures
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Ans ; Inj sodium valproate and Inj phenytoin have anti platlet activity
3. Cardiology :
A) Link to patient details:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
ANS: The amount of blood pumped out of the heart with each beat is called the ejection fraction (EF). A normal EF is usually around 55 to 70 percent, but it can be lessened in some forms of heart failure.-People with heart failure with reduced ejection fraction (HFrEF) have an EF that is 40 to 50 percent or lower. This is also called systolic heart failure. People with heart failure with preserved ejection fraction (HFpEF) do not have much of a change in their ejection fraction. This is often called diastolic heart failure.
-HFrEF were often diagnosed earlier in life and right after a heart attack.
HFpEF were diagnosed later in life and first experienced symptoms of heart failure between the ages of 65 and 69. Many of those with HFpEF also shared that they have other health problems that led to their diagnosis. Many of them also live with additional health conditions, including acid reflux (GERD), high blood pressure, kidney disease, and sleep disorders.
-HFrEF shared that they feel depressed and/or anxious about their heart failure diagnosis. Risk factors for those in this group include genetics or a family history of heart failure.
HFpEF shared that they are still able to do the things they enjoyed before their heart failure diagnosis.risk factors, including:
Sedentary lifestyle
High blood pressure
Sleep apnea
Other heart conditions
-HFrEF are more likely to have had surgery, including surgery to implant a pacemaker or other heart rhythm control device.HFrEF shared that they currently use a combination therapy to treat their heart failure.
HFpEF have never had surgery to treat their heart failure or had a device implanted.
-HFrEF are men who live in rural areas.
However, most respondents with HFpEF are women who live in urban areas.
2.Why haven't we done pericardiocenetis in this pateint?
ANS;
Pericardiocentesis is done when the pericardial effusion is not resolving on its own . Here the pericardial fluid which has accumulated was resolving on its own , at the time of admission it was 2.4mm and when discharged it was 1.9 mm . Therefore we did not do pericardiocentesis in this pt.
3.What are the risk factors for development of heart failure in the patient?
ANS: IN THIS PATIENT:
NON MODIFICABLE:
age
gender
MODIFIABLE:
hypertension
smoking
type 2 diabetes .
kidney disease.
4.What could be the cause for hypotension in this patient?
ANS:
The pt. was anemic with Hb of 8gm/dl . One of the severe complication of anemia is tissue hypoxia which further lead to hypotension. B) Link to patient details
1.What are the possible causes for heart failure in this patient?
ANS:
Obesity
alcohol
diabetes
hypertension
2.what is the reason for anemia in this case?
ANS: Alcoholics frequently have defective red blood cells that are destroyed prematurely, possibly resulting in anemia. Alcohol also interferes with the production and function of white blood cells, especially those that defend the body against invading bacteria. Consequently, alcoholics frequently suffer from bacterial infections.
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
ANS:
The pt. had recurrent blebs and ulcer on lower limbs (foot). This is due to Type to diabetes mellitus.
Diabetic foot ulcers generally arise as a result of poor circulation in the foot region. While high blood sugar levels and nerve damage or even wounds in the feet may result in foot ulcers in many cases.
In cases of poor circulation of blood, the foot ulcers take quite a bit of time to heal as the blood efficiency in the foot region is at a low level. Furthermore, many develop a bit of reduced sensation on the feet as a result of nerve damage or more.
There are many risk factors that may lead to foot ulcers at the end.
Poor quality or fitting of the footwear.
Unhygienic appearance of foot.
Improper care of the nails of the toe.
Heavy intake of alcohols and tobacco.
Obesity and Weight-related
Complication arising from Diabetes like eye problems, kidney problems and more.
Although aging or old age can also be counted among them.
4. What sequence of stages of diabetes has been noted in this patient?
ANS: alcohol------obesity------impaired glucose tolerance------diabetes mellitus------microvascular complications like triopathy and diabetic foot ulcer-------macrovascular complications like coronary artery disease , coronary vascular disease and peripheral vascular disease. 1Q) what is the evolution of the symptomatology in this patient interms of an event timeline and where is the anatomical localisation for the problem and what is the primary etiology of the patient problem ?
C) Link to patient details:
https://preityarlagadda.blogspot.com/2021/05/biatrial-thrombus-in-52yr-old-male.html
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans:Patient was apparently asymptomatic 2 days ago when he developed Shortness of breath Grade II (on exertion) which progressed to Grade IV (at rest) for which he visited local RMP and was referred to our hospital.Patient also complains of decreased urine output since 2 days and Anuria since morning.
Anatomical localization is heart
Primary etiology is atrial fibrillation
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans; 1) INJ. Dobutamine 3.6ml/hr was given to maintain the falling BP up to a MAP of 55 mmHg.
Mechanism of action: Dobutamine is a direct-acting inotropic agent whose primary activity results from stimulation of the ß receptors of the heart while producing comparatively mild chronotropic, hypertensive, arrhythmogenic, and vasodilative effects. It does not cause the release of endogenous norepinephrine, as does dopamine
.2) TAB. Digoxin 0.25mg OD 5/7 and INJ. Unfractionated Heparin 5000 IU TID.
Mechanism of action: Digoxin has two principal mechanisms of action which are selectively employed depending on the indication: Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump, an enzyme that controls the movement of ions into the heart
3[INJ. Unfractionated Heparin Infusion @5ml/hr
Mechanism of action: It produces its major anticoagulant effect by inactivating thrombin and activated factor X (factor Xa) through an antithrombin (AT)-dependent mechanism. ... By inactivating thrombin, heparin not only prevents fibrin formation but also inhibits thrombin-induced activation of platelets and of factors V and VIII.Other medications used during the course in hospital -
1. TAB. Cardivas3.125mg PO/BD
2. TAB. Dytor 10mg PO/OD
3. TAB Pan D 40mg PO/OD
4. TAB. Taxim 200mg PO/OD
5. INJ. Thiamine 100mg in 50ml NS IV/TID
6. INJ. HAI S.C 8U-8U-6U
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
Ans; The pathophysiology of CRS can be attributed to two broad categories of "hemodynamic factors" such as low cardiac output, elevation of both intra-abdominal and central venous pressures, and non-hemodynamic factors or "cardiorenal connectors" such as neurohormonal and inflammatory activation.[5] It was previously believed that low cardiac output in heart failure patients result in decreased blood flow to the kidneys which can lead to progressive deterioration of kidney function. As a result, diuresis of these patients will result in hypovolemia and pre-renal azotemia.
In addition, CRS has been observed in patients with diastolic dysfunction who have normal left ventricular systolic function.[3]Therefore, there must be additional mechanisms involved in the progression of CRS. Elevated intra-abdominal pressures resulting from ascites and abdominal wall edema may be associated with worsening kidney functions in heart failure patients. Several studies have shown that as a result of this increased intra-abdominal pressure there is increased central venous pressure and congestion of the kidneys' veins, which can lead to worsening kidney function.[3]
In addition, many neurohormonal and inflammatory agents are implicated in the progression of CRS. These include increased formation of reactive oxygen species, endothelin, arginine vasopressin, and excessive sympathetic activity which can result in myocardial hypertrophy and necrosis.
Other cardiorenal connectors include renin-angiotensin-system activation, nitric oxide/reactive oxygen species imbalance, inflammatory factors and abnormal activation of the sympathetic nervous system, which can cause structural and functional abnormalities in both heart and/or the kidney. There is a close interaction within these cardiorenal connectors as well as between these factors and the hemodynamic factors which makes the study of CRS pathophysiology complicated.
4) What are the risk factors for atherosclerosis in this patien
Ans; High cholesterol and triglyceride levels.
High blood pressure.
Smoking.
Type 1 diabetes.
Obesity.
Physical inactivity.
High saturated fat diet.t?
5) Why was the patient asked to get those APTT, INR tests for review?
Ans; Standard coagulation screening tests such as activated partial thromboplastin time (APTT), prothrombin time (PT), and the international normalized ratio (INR) are important constituents of basic examinations in clinical laboratories. APTT can be used as an indicator of intrinsic coagulation pathway activity, and a short APTT is linked to increased thrombin generation and increased risk for thrombosis.
D) Link to patient details: https://daddalavineeshachowdary.blogspot.com/2021/05/67-year-old-patient-with-acute-coronary.html?m=1
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
TIMELINE OF EVENTS-
• Diabetes since 12 years - on medication
• Heart burn like episodes since an year- relieved without medication
• Diagnosed with pulmonary TB 7 months ago- completed full course of treatment, presently sputum negative.
• Hypertension since 6 months - on medication
• Patient presented with Shortness of Breath
Anatomical localisation - Cardiovascular system
Etiology: The patient is both Hypertensive and diabetic and these may result in the development of atherosclerosis.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Pharmacological interventions:
TAB MET XL 25 MG/STAT-contains Metoprolol as active ingredient
MOA: METOPROLOL is a cardiselective beta blocker
Beta blockers work by blocking the effects of the hormone epinephrine. Beta blockers have a negative chronotropic effect
and negative inotropic effect.
Beta blockers also have antiarrhythmic effects and also anti ischemic effects. They also inhibit renin.
EFFICACY STUDIES.
In CAD, 12 meta-analyses (93 RCTs, 103,481 patients) showed that beta-blockers reduced mortality in analyses before routine reperfusion, but there was a lack of benefit in contemporary studies where ≥ 50% of patients received thrombolytics or intervention.
Non pharmacological intervention advised to this patient is: PERCUTANEOUS CORONARY INTERVENTION.
Percutaneous Coronary Intervention is a non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup ( atherosclerosis).
3) What are the indications and contraindications for PCI?
INDICATIONS and CONTRAINDICATIONS:
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
Although PCI is generally a safe procedure , it might cause serious certain complications like
A)Bleeding
B) Blood vessel damage
C) Allergic reaction to the contrast dye used
D) Arrhythmias
E) Need for emergency coronary artery bypass grafting .
⁃ OVER TESTING AND OVER TREATMENT :
In olden days doctors would so much depend on their intuition as technology was not available .But these days every physician is dependent on laboratory reports.We cannot say it is a bad thing as it would lead to accurate diagnosis, but the point is these should be used logically only where they are required.Or else it would lead to overtesting.And overtesting has its own adverse effects.For example during the recent 2nd wave of Covid Pandemic majority of the Covid Patients including the asymptomatic and patients with mild disease were advised to take CT Scan which lead to unwanted radiation exposure.Even overtreatment has its own adverse effects.So even though all the Therapeutic and Diagnostic Facilities are available at our disposal , Physicians should use them Judiciously or Else they will do more harm than good. E) Link to patient details:
https://bhavaniv.blogspot.com/2021/05/case-discussion-on-myocardial-infarction.html?m=1
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans;Evolution of symptomatology:
Uncontrolled DM2 since 8 years
3 days back Mild chest pain dragging type and retrosternal pain(radiated)
Anatomical localisation: Inferior wall of heart
Primary etiology: Diabetes type 2 (uncontrolled)
high blood glucose from diabetes can damage your blood vessels and the nerves that control your heart and blood vessels
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans;TAB. ASPIRIN 325 mg PO/STAT
Mechanism of action: The acetyl group of acetylsalicylic acid binds with a serine residue of the cyclooxygenase-1 (COX-1) enzyme, leading to irreversible inhibition. This prevents the production of pain-causing prostaglandins.
TAB ATORVAS 80mg PO/STAT
Mechanism of action: Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver.
TAB CLOPIBB 300mg PO/STAT
Mechanism of action: The active metabolite of clopidogrelselectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
INJ HAI 6U/IV STAT
VITAL MONITORING.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Ans; Repeat PTCA provides a valuable, safe and cost-effective way of management for recurrence of stenosis after initially successful angioplasty. It increased the percent of patients with documented long-term success of angioplasty
Over testing and over treatment can raise a person’s risk of cardiovascular death by as much as four times.
F) Link to patient details:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
Because of the fluid lossoccured to the patient
There is
Decreased preload → SOB occured due to decreased cardiac output
IV fluids administered → there is increase in preload → SOB decreased due to better cardiac output
2. What is the rationale of using torsemide in this patient?
Torsemide is used due to abdominal distension
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
Treatment for UTI
Rationale - used for any bacterial infection .
4.Gastroenterology and pulmonology:
A.LINK TO PATIENT DETAILS:
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-pancreatitis-with.html
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Evolution of symptomatology
H5 years back-1st episode of pain abdomen and vomitings
Stopped taking alcohol for 3 years
1 year back 5 to 6 episodes of pain abdomen and vomitings after starting to drink alcohol again
20 days back increased consumption of toddy intake
Since 1 week pain abdomen and vomiting
Since 4 days fever constipation and burning micturition
Anatomical localisation: Pancreas and left lung
Alcohol and its metabolites produce changes in the acinar cells, which may promote premature intracellular digestive enzyme activation thereby predisposing the gland to autodigestive injury. Pancreatic stellate cells (PSCs) are activated directly by alcohol and its metabolites and also by cytokines and growth factors released during alcohol-induced pancreatic necroinflammation. Activated PSCs are the key cells responsible for producing the fibrosis of alcoholic chronic pancreatitis
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A) * Non pharmacological interventions : drains ( malecot & icd )
* Even i as a treating physician will follow the same approach
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
B) Link to patient details:
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-25-year-old-male.html
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
*pleural effusion is cause for patients dyspnea.
*pleural effusion may occur due to pancreaticopleural fistulae secondary to leak and disruption of pancreatic duct .
2) Name possible reasons why the patient has developed a state of hyperglycemia.
* Hyperglycemia is developed due to abnormalities in insulin secretion , increase in counter regulatory hormone release ,decreased utilization of glucose by peripheral tissue.
Exocrine pancreatic dysfunction impairs the endocrine pancreas.
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
*
4) What is the line of treatment in this patient?
* iv fluids and colloids to maintain normal intravascular volume.
*Nil orally
*Analgesics for pain relief
*Nasogastric suction -to decrease gastrin release from stomach
* Monitor
-BP, pulse,blood sugars ,serum amylase, serum lipase ,urine output.
* laparotomy and debridement of hemorrhagic pancreatic tissue.
* antibiotic therapy like ciprofloxacin , ofloxacin, imipenem
C) Link to patient details:
https://chennabhavana.blogspot.com/2021/05/general-medicine-case-discussion-1.html
1) What is the most probable diagnosis in this patient?
àDifferential Diagnosis:
· Ruptured Liver Abscess.
· Organized collection secondary to Hollow viscous Perforation.
· Organized Intraperitoneal Hematoma.
· Free fluid with internal echoes in Bilateral in the Subdiaphragmatic space.
· Grade 3 RPD of right Kidney
àThe most probably diagnosis is there is abdominal hemorrhage. This will give reasoning to the abdominal distention, and the blood which is aspirated.
2) What was the cause of her death?
àAfter leaving the hospital, the patient went to Hyderabad and underwent an emergency laparotomy surgery. The patient passed away the next day. Cause of her death can be due to complications of laparotomy surgery such as, hemorrhage (bleeding), infection, or damage to internal organs.
3) Does her NSAID abuse have something to do with her condition? How?
àNSAID-induced renal dysfunction has a wide spectrum of negative effects, including decreased glomerular perfusion, decreased glomerular filtration rate, and acute renal failure. Chronic NSAIDs use has also been related to hepatotoxicity. While the major adverse effects of NSAIDs such as gastrointestinal mucosa injury are well known, NSAIDs have also been associated with hepatic side effects ranging from asymptomatic elevations in serum aminotransferase levels and hepatitis with jaundice to fulminant liver failure and death
5.Nephrology and urology:
A.LINK TO PATIENT DETAILS:
https://kavyasamudrala.blogspot.com/2021/05/medicine-case-discussion-this-is-online.html
1) What could be the reason for SOB??
As the patient was administered diuretics may be it has lead to increased excretion of Bicarbonate ions.So there will be Metabolic Acidosis.To compensate that there will be increase in the respiratory rate to eliminate the CO2 so that equilibrium is maintained.Hence there will be Shortness of Breath due to increased respiratory rate.
2) Why does he have intermittent episodes of drowsiness??
Use of Diuretics has lead to Hyponatremia which resulted in Drowsiness.
3)Why did he complain of fleshy mass like passage in urine ??
There are large no. Of puss cells in his urine.May be the patient confused these with a fleshy Mass.
4)What are the complications of TURP that he may have had ??
TURP -Transurethral resection of Prostate
- May be Glycerol used for bladder wash during the procedure has caused some damage to the kidney.There was a rise in his creatinine levels following the procedure.
There is also chance of infection.
Patient's WBC count is also Raised. B) Link to patient details:
1.Why is the child excessively hyperactive without much of social etiquettes ?
1ans* The exact pathophysiology of Attention Deficit Hyperactivity Disorder (ADHD) is not clear. With this said, several mechanisms have been proposed as factors associated with the condition. These include abnormalities in the functioning of neurotransmitters, brain structure and cognitive function.
* Due to the efficacy of medications such as psychostimulants and noradrenergic tricyclics in the treatment of ADHD, neurotransmitters such as dopamine and noradrenaline have been suggested as key players in the pathophysiology of ADHD.
* Depressed dopamine activity has been associated with the condition,
2. Why doesn't the child have the excessive urge of urination at night time ?
2ans:the child doesn’t have the excessive urge of urination at night time because ADHD is a physcosomatic disorder
3. How would you want to manage the patient to relieve him of his symptoms
TREATMENT
Amphetamine which is a CNS stimulant will be useful in this Patient.
I would also try to change the Parenting Behaviour and teach the parents Positive Reinforcement Methods so that the child would get A Good Family Support.
Cognitive Training should also be Given to the child.
6.Infectious diseases:
A.LINK TO PATIENT DETAILS:
A) https://vyshnavikonakalla.blogspot.com/2021/05/a-40-year-old-lady-with-dysphagia-fever.html
Q) 1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
Laryngeal Crepitus,Difficulty in swallowing initially to the solids,
Cough,are Suggestive of TracheoEsophageal Fistula.
Q) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
Risk Factors For Development of Immune Reconstitution Inflammatory Syndrome (I R I S)
1) Low Baseline CD4 Count
2) Higher Baseline Viral Load
3) Shorter Interval between commencing ATT and HAART
4) Disseminated TB
5) A Greater Decrease in Viral Load after starting HAART.
As this patient has a low baseline CD4 count and also disseminated TB there are chances that this patient may develop IRIS.
If the following symptoms are seen after the Initiation of ART then IRIS can be suspected
1) Fever,Anemia,Wt loss.
2) CNS
3) Lymphadenopathy
4) Radiological Findings
5) Exacerbation of Pulm. Lesion or occurence Of a new Lesion.
Prevention of IRIS :
CD4+ T cell deficiency when ART is commenced is a risk factor for an IRIS, prevention of CD4+ T cell depletion through early diagnosis and treatment of HIV infection regardless of CD4+ T cell count, as supported by the findings of the START study (33), is the most effective measure for reducing the risk of developing an IRIS.
However, 'late presenters' with advanced immunodeficiency continue to present and they must be assessed carefully for HIV-related infections that might trigger an IRIS when ART is commenced.
7.infections disease and hepatology:
A.Link to patient details:
1) Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ??
Yes, may be the liver Abcess developed due to the chronic intake of contminated Toddy.
2) What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
Chronic alcohol intake especially the locally available contaminated drinks plays a major role in the formation of liver abscesses which can be either Amoebic or Pyogenic liver abscess because of the adverse effects of alcohol over the Liver.
3) Is Liver Abcess more common in Right Lobe ??
50% of solitary liver abscesses occur in the right lobe of the liver (a more significant part with more blood supply), less commonly in the left liver lobe or caudate lobe.
4) what are the indications of Ultrasound-guided aspiration of Liver abscess ?
Indications for USG guided aspiration of liver abscess
1. Large abscess more than 6cms
2. Left lobe abscess
3.Caudate lobe abscess
4. Abscess which is not responding to drugs
B.LINK TO PATIENT DETAILS:
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-liver-abcess.html
1) Cause of liver Abcess in this Patient??
May be due to malnutrition and lack of personal hygeine is the cause of the infection in the patient resulting in liver abcess. The infection may be amoebic or any other bacterial infection.
2) How do you approach this Patient??
As the patient presented with the pain in the abdomen, first I would go for a USG abdomen and As USG showing hyperechoic mass on the liver I would also do LFT(Liverfunction Test)
As there is a mass as seen in USG and LFT is also abnormal (Raised ALP), I would start empirical Treatment for both Amoebic and pyogenic liver abscess.
According to the response given to this Medical Treatment it will be decided whether aspiration is required or not. 8.infectious diseases( mucormycosis,ophthalmology)
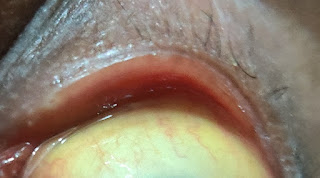
A) http://manikaraovinay.blogspot.com/2021/05/50male-came-in-altered-sensorium.html1) QUESTION: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
1. 3 years ago diagnosed with hypertension
2. 21 days ago he received vaccination at local PHC which was followed by fever associated with chills and rigors, high grade fever.
3. 18 days ago he complained of similar events and went to the the local hospital, it was not subsided upon taking medication.
4. 11 days ago he complained of Generalized weakness and facial puffiness and periorbital oedema. Patient was in a drowsy state
5. 4 days ago-
a. patient presented to casualty in altered state with facial puffiness and periorbital oedema and weakness of right upper limb and lower limb
b. towards the evening patient periorbital oedema progressed
c. serous discharge from the left eye that was blood tinged
d. was diagnosed with diabetes mellitus
6. patient was referred to a government general hospital
7. patient died 2 days ago
Patient wasn't aware of his diabetic condition until then. He was also suffering from diabetic acidosis.This resulted in poorly controlled blood sugar levels. The patient was diagnosed with acute rhinocerebral mucormycosis. Rhino cerebral mucormycosis is the most common form of this fungal disease that occurs in people with uncontrolled diabetes.The fungus enters the sinuses from the environment and then the brain.
The patient was also diagnosed with acute infarct in the left frontal and temporal lobe. Mucormycosis is associated with the occurrence of CVA
2) QUESTION: What is the efficacy of drugs used along with other non-pharmacological treatment modalities and how would you approach this patient as a treating physician?
The proposed management of the patient was –
1. inj. Liposomal amphotericin B according to creatinine clearance
2. 200mg Iitraconazole was given as it was the only available drug which was adjusted to his creatinine clearance
Management of diabetic ketoacidosis –
a) Fluid replacement- The fluids will replace those lost through excessive urination, as well as help dilute the excess sugar in blood.
(b) Electrolyte replacement-The absence of insulin can lower the level of several electrolytes in blood. Patient will receive electrolytes through a vein to help keep the heart, muscles and nerve cells functioning normally.
(c) Insulin therapy- Insulin reverses the processes that cause diabetic ketoacidosis. In addition to fluids and electrolytes, patient will receive insulin therapy
Granulocyte stimulating factors may also be used in the treatment of mucormycosis.
Hyperbaric oxygen can also be used as an adjunctive therapy.
3) QUESTION: What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
I think it is because of the use steroids in an uncontrolled manner.
COVID 19 is not the first disease where steroids are used as one of the main stay of treatment (in severe cases) but what has gone wrong in the recent time is even the lay man who got infected with Corona started using steroids right from the day 1 with no monitoring by a specialised physician.And they are not following any specific course of treatment.As many of them are also diabetic patients the are getting succumbed to mucormycosis.And it is not ending with mucormycosis but various other fungii are emerging to cause an epidemic.
And another reason for rise in mucormycosis cases may be the usage of tap water in oxygen concentrators.As most of the patients are being diagnosed of Covid in late stages in the second wave many of them Are requiring oxygen concentrators for supplemental oxygenation.And due to Lack of the people are using tap water instead of distilled water which serves as reservoir for the growth of mucormycosis.So this may be one of the reason for rise in mucormycosis cases.