35 year old male came with C/o occasional palpitations and SOB since 3 months.
35 year old male came with C/o occasional palpitations and SOB since 3 months.
June 04, 2023
This is an online elog documenting de-identified patient health data after taking his signed consent to enforce a greater patient centered learning.
DEIDENTIFICATION -
The privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
CASE DISCUSSION -
35 year old male came with C/o occasional palpitations and SOB since 3 months.
HOPI-
Patient was apparently asymptomatic 3 months back, then started developing occasional palpitations, relieved on consuming alcohol, not a/w chest pain.
He developed SOB since 3 months, Grade 2, insidious in onset, gradually progressive, no aggravating and relieving factors.
C/o decreased appetite since 2 months.
C/o generalised weakness since 10 days.
No H/o orthopnea and PND.
No C/o fever, decreased urine output, burning micturition, pedal edema.
PAST HISTORY-
Not a k/c/o DM, HTN, CVA, CAD, TB, Epilepsy.
PERSONAL HISTORY-
Addictions- Patient is a regular drinker since last 15-16 yrs, drank 180mL whisky every evening.
Then 5 months back had sudden resistance to alcohol, started feeling disgusted even at the sight of alcohol so he left alcohol for 1 month.
After 1 month he started developing tremors, palpitations which subsided on drinking, so gradually started drinking more, currently drinking 360mL to 540mL of whisky daily.
No other addictions.
Appetite- Decreased
Diet: Mixed
Sleep: Adequate
Bowel and bladder movements: Regular
Family History:
Not significant.
General Examination -
Patient is examined in a well lit room with adequate exposure, after taking the consent of the patient.
He is conscious, coherent and cooperative.
Built & nourishment-Moderate
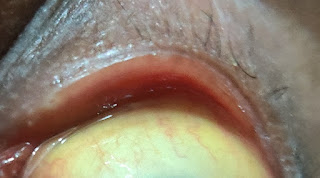
Icterus - Present
No pallor
No cyanosis
No clubbing
No edema
No lymphadenopathy.
Vitals:
Temp: 98.1 F
Bp: 130/90 mmHg
PR: 106 bpm
RR: 20 cpm
SpO2: 98% on RA
GRBS: 164 mg%
Systemic Examination -
CVS :
S1 S2 present
No murmurs
RESPIRATORY SYSTEM;
B/l symmetrical chest
Trachea - Central
B/l air entry present
NVBS heard
ABDOMEN:
Shape of abdomen: Obese
Soft, non tender.
No rigidity or guarding.
CNS :
NFND, HMF intact
Reflexes - Normal
Investigations:


.jpg)








